As with many academic medical health systems across the country, Yale New Haven Health (YNHH) has grown through the integration of regional hospitals to deliver state of the art patient care directly to communities across Connecticut and southwestern Rhode Island. The integration of a regional or community health provider into a larger health care system, like Yale New Haven Health, includes a complex process of research, relationship building, and negotiation. To meet the patient care and clinical goals that Yale New Haven Health hopes to achieve by integrating a regional hospital system like Lawrence + Memorial Hospital, they need to understand the state of the facilities and physical plant that supports the hospital.
In this three-part series, we will discuss the planning, design and construction process that has supported Lawrence + Memorial Hospital in New London, CT, through their integration into the Yale New Haven Health System.

Phase 1: Identification of the Facility
Early relationship building is essential in the integration of a regional hospital into a healthcare network. Before any facilities or design teams are brought on board, YNHH establishes relationships with potential regional hospitals, state and regulatory agencies and other key stakeholders. Creating these relationships early on helps to clearly understand the benefits that YNHH can bring to the patients, community and staff supporting the existing facility.
This first phase focuses on clinical, patient care needs and goals both from the perspective of the regional hospital and the health system. Review of patient volumes, demographics, clinical specialties, the balance of services across the health system and market opportunities are all parts of this phase that do not yet involve Facilities, Design and Construction.
Phase 2: Due Diligence
Once a facility has been identified, and the integration process has begun, the understanding of existing facilities becomes increasingly essential. Once the facility design, planning and construction become the focus of the regional hospital integration process, there are some critical early steps that YNHH implements are each hospital campus:
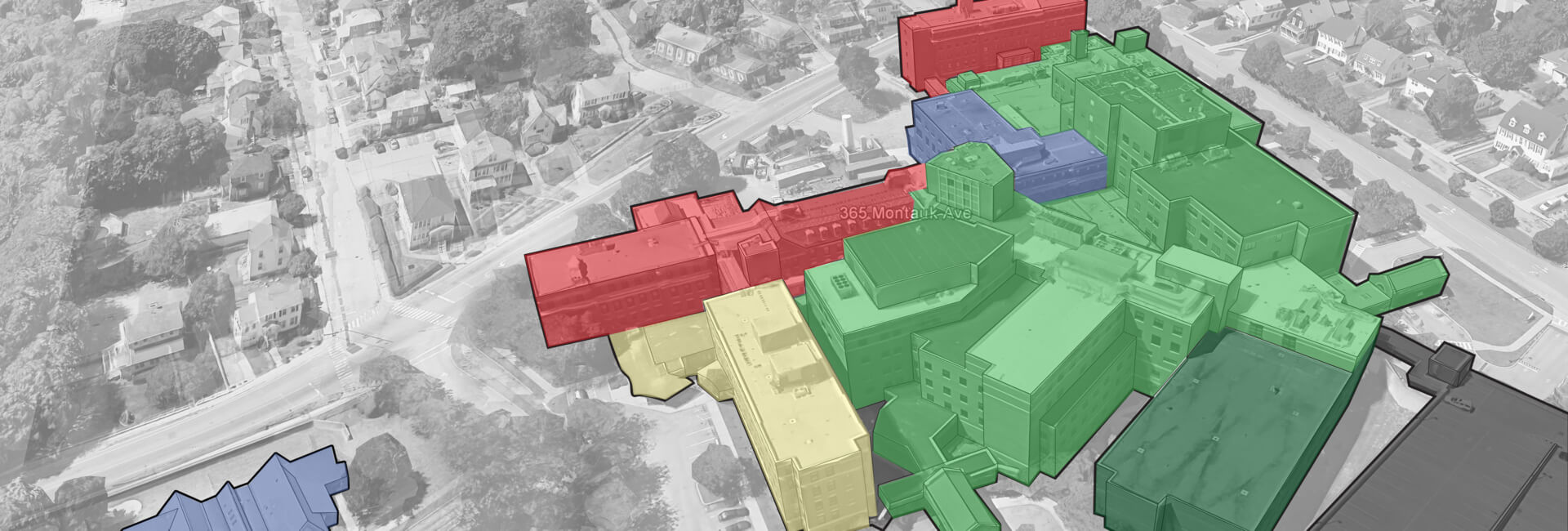
Dedicated Design Team: A dedicated design team is engaged for each hospital campus that is part of the YNHH system. For Lawrence + Memorial Hospital, both PAYETTE and BR+A were engaged to establish a knowledge base of the campus through site visits, field surveys and discussions with existing facility staff. Once several projects reach implementation, the design team will have already developed a coherent design language and history at the hospital that allows for more efficient project planning and execution. Understanding of infrastructure capacity and deferred maintenance needs are of particular importance when building the design team’s knowledge base. With each new renovation project at Lawrence + Memorial Hospital, PAYETTE and BR+A can evaluate options based not only on programmatic needs but on whether infrastructure upgrades are needed to support the type of program proposed.
Seven-year look ahead capital planning: Developing a strategic capital plan allows financial leadership to understand the order of magnitude funding required to support the capital improvement for the integrated regional hospital. As well, it helps to illustrate when more substantial outlays of funding will be necessary for more extensive infrastructure upgrades, equipment replacements, or renovation projects. The capital plan is a live document that is updated each year, supported by a Facility Assessment and Strategic Masterplan. YNHH Facilities Design and Construction maintains a capital plan on a seven-year time timeline as it is easily understandable by all parties involved in financial decision making.
Facility Assessment and Strategic Master Planning: For each hospital campus, YNHH commissions a facility assessment report as a first step in understanding the physical plant of a hospital similar to Lawrence + Memorial Hospital. The Facility Assessment is intended to answer several key questions:
- What deferred maintenance is there?
- What infrastructure capacity is available and how does it compare to the current needs of the facility as well as potential future needs?
- What is the highest and best use of each building in facility both in terms of investment needed in the physical plant and how those buildings best meet clinical and programmatic needs?
- What opportunities are available for improving the facility in the near, middle, and long-term horizons?
- Strategic Master Plan follows each Facility Assessment to provide the regional hospital and health care system with options for how to meet both clinical and patient care goals and address facility needs.
The next part of this series will address the Facility Assessment and Strategic Master Planning process in greater detail.
Acknowledgements:
Mario Vieira, AIA, Executive Director Facilities Design Construction, Yale New Haven Health
Steve Levin, Principal, BR+A Consulting Engineers
Kevin Ledoux, Associate Principal, Electrical Engineer, BR+A Consulting Engineers
Robert Rose, PE, Vice President, A-Z Corporation
Related Links:
Improving Emergency Department Patient Flow
PAYETTE People at NEHES Conference