Part 2 of our series on the Integration of Regional Hospitals into Healthcare Networks takes a more in-depth look at the critical Facility Assessment and Strategic Master Planning phase of the integration process. This phase of planning sets the requirements for the seven-year capital plan described in Part 1 that facilitates real project implementation that is the ultimate goal of all planning projects.
Phase 3: Facility Assessment and Strategic Master Planning
At many regional hospitals, when capital resources become more constrained, priority is given to improvement projects that have direct clinical improvement outcomes. This often comes at the expense of infrastructure-related projects that, while important, do not have the same kind of visible results from a patient care perspective, until that infrastructure fails or becomes critical. To understand the deferred maintenance and state of the physical plant at Lawrence + Memorial Hospital, PAYETTE and BR+A developed a facility assessment to review:
Existing documentation: With limited facilities staff, maintaining plan archives and existing conditions, documentation is often put on the back burner to address immediate facility needs. When PAYETTE and BR+A began the Facility Assessment at Lawrence + Memorial Hospital in 2017, the latest available facilities documentation for the hospital dated from 2015. Even in the intervening two years, staff moves and renovations had made some of that documentation obsolete. In order to move forward with the integration, a comprehensive life safety statement of conditions report was included in the L+M Facility Assessment to give the YNHH a baseline understanding of the current facility conditions on which they would be building.
Exterior building envelope assessment: All elements of the exterior building envelope were evaluated for existing wear and maintenance including the windows, doors, masonry, facades, roofs, etc. Facilities staff with historical knowledge of the physical plant and day to day knowledge of building maintenance were essential in identifying timelines of recent upgrades and locations where critical deferred maintenance is present. Each exterior envelope element was assigned near term, medium-term and long-term requirements for maintenance and upgrades. Medium to long term projects typically become activated when renovation projects to support clinical or infrastructure needs impact those elements of the exterior envelope.

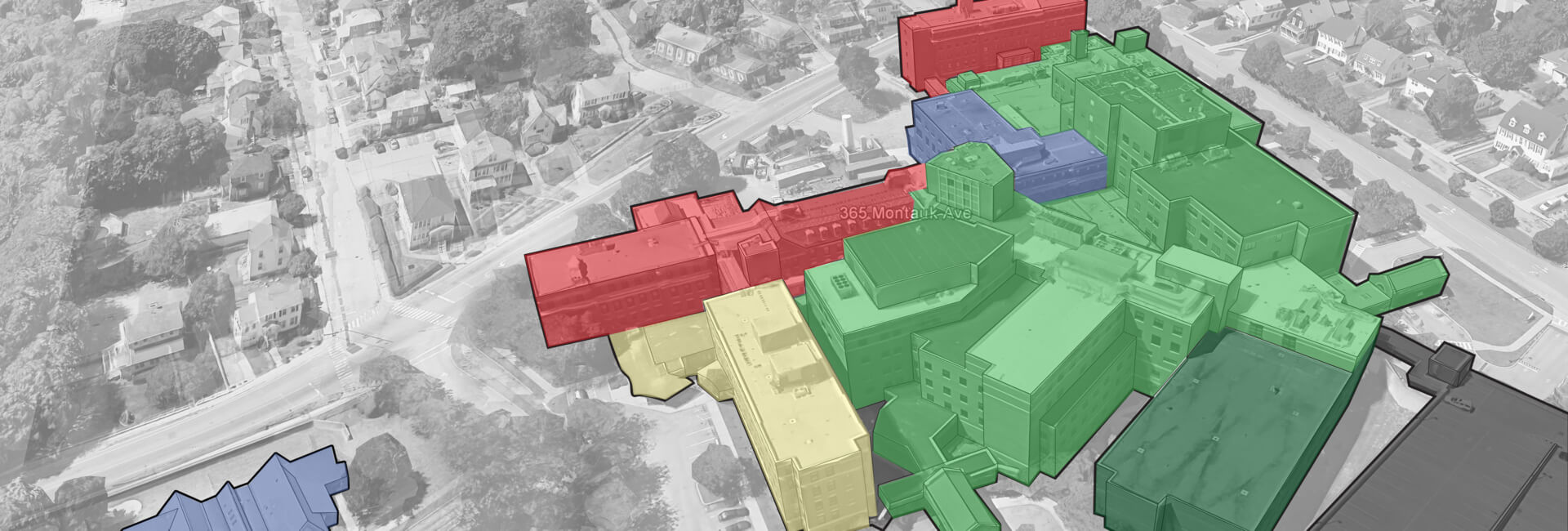
Interior assessment: Evaluation of existing interior conditions and materials is part of the interior component of the Facility Assessment. However, the interior portion of the Facility Assessment should go beyond these elements to evaluate the internal planning and structure of each building to determine its highest and best use. PAYETTE’s interior assessment of Lawrence + Memorial Hospital included:
• Departmental program adjacencies
• Analysis of floor to floor heights and structural bays: are the programs in the existing buildings suited to the buildings that house them?
A key finding from the Facility Assessment at L+M highlighted the Ambulatory Care Center, which had been constructed as a B-occupancy ambulatory care building. As a result, the use of that building is limited to outpatient functions and cannot house I-occupancy functions in the future by code.
Infrastructure assessment: Understanding deferred maintenance and capacity of existing infrastructure is a critical part of a Facility Assessment. The Facility Assessment should focus on high-level infrastructure capacity, systems and equipment – the “heart” or “brains” of the systems instead of the “arteries” or “nerves.” As well, it is important to understand that smaller-scale infrastructure issues are easier to fix as part of renovation projects. Extensive infrastructure replacements or upgrades have capital cost implications that need to be understood upfront. One of the critical infrastructure challenges identified at Lawrence + Memorial Hospital was the safety, redundancy and capacity of the standard and emergency electrical systems.
YNHH commissions a Facility Assessment as early in the integration process as possible to understand what the critical facility needs are from the outset. Strategic master planning, on the other hand, follows the Facility Assessment with an interim period of about a year after the integration of the regional hospital. Most regional hospital integration into a more extensive healthcare network involves a leadership change at the regional level. Those new leaders need time to become embedded into the regional hospital, to establish their own goals and priorities on the clinical and administrative side before those goals can be applied to a strategic master plan.
The strategic master plan is where clinical goals and facility needs overlap, and opportunities can be identified to address both clinical needs, and facility infrastructure and deferred maintenance needs together. By going through the strategic master planning process, high-level stakeholders both at the regional hospital and the healthcare system will have a better understanding and realistic expectations about the timelines and efforts involved in upgrading hospital facilities. Having a road map for facility design and construction helps to manage user expectations. For example, having a clear plan helps to provide clarity regarding how quickly facility changes may be able to address clinical processes and patient care needs. As well, it makes it easier to identify and manage whatever infrastructure changes are needed to support clinical space renovations.
It’s important to note that a strategic master plan is not a set-in-stone document and should be revisited as the hospital identifies new needs and new projects develop. It is most useful if the plan outlines a set of options that sorts levels of intervention in the hospital based on short-term, medium-term and long-term priorities. By determining the different priority levels, it gives the healthcare provider/ hospital options and a variety of paths to meet their goals. A key outcome of a strategic master plan is a list of priorities that ties into the seven-year capital plan described earlier. Tying the strategic master plan and capital plan together in this way makes it more likely that projects outlined in the master plan will have appropriate funding to be achieved on the hospital’s desired timeline.
The last part of this series will highlight the Emergency Department Expansion and Emergency Power Improvement project, which is the first major clinical and infrastructure project undertaken at Lawrence + Memorial Hospital since it joined the Yale New Haven Health System.
Acknowledgements:
Mario Vieira, AIA, Executive Director Facilities Design Construction, Yale New Haven Health
Steve Levin, Principal, BR+A Consulting Engineers
Kevin Ledoux, Associate Principal, Electrical Engineer, BR+A Consulting Engineers
Robert Rose, PE, Vice President, A-Z Corporation
Related Links:
Integration of Regional Hospitals into Healthcare Networks: Health System Planning
PAYETTE People at NEHES Conference
Improving Emergency Department Patient Flow