In this series, members of our core healthcare team discuss design philosophy and current trends in healthcare design.

Dartmouth-Hitchcock Medical Center, Center for Surgical Innovation
The healthcare industry is in almost an intense state of flux with no end in sight for the foreseeable future. Our own medical successes drive this “environment for change.” Advancements in medical care, pharmaceuticals and medical technology, along with the mass transfer of information, have created a “great day” for patients who, only 20 years ago, would have been looking at far different outcomes. While it is hard to see this advancement and the speed at which we continue to progress as a problem, the environment we have strived to develop has created new challenges for campus and facility design.
As we progress, the volume of outpatient care will increase significantly, and while inpatient volume overall will decrease, the sick will get sicker. Technology will continue to advance at extreme rates, but this requires the need to upgrade, replace and support equipment we cannot even fathom five to ten years after opening a new facility. Our caregivers will have the most advanced tools and best education, but the volume of patients that can be treated and the levels of care required at the tertiary centers will drive a much higher level of stress. The future of healthcare is bright, and healthcare architecture and planning is rushing to adapt.
Overall, there are six elements which, for now, must be considered when planning health campuses, systems and facilities for the future of healthcare delivery: flexibility, technology-led design, role of design in a provider of choice environment, higher acuity levels in more facilities, growing outpatient care and facility repurposing.
Flexibility
Flexibility will need to be the overarching driver for any campus planning engagement or building design. Facilities are expensive and will become more so in the future. Investments will be substantial and an institution’s ability to constantly renovate, due to changing equipment or medical processes, will be limited. Our ability to provide physical solutions that can adapt will be paramount to the financial viability of a system. This level of flexibility will need to exist on multiple levels. Individual treatment rooms will need to have adaptable technology. Structural systems will need to be able to accept new technology, new layouts and advanced security. Mechanical systems will need to be able to adapt to security risks, zone off for isolation and remain operational during a number of different internal scenarios. Data system, primarily the information backbone, will need to be robust, accessible and upgradable. Beyond the physical flexibility of individual areas, the operational adaptability of a space will be more crucial. A facility’s ability to handle multiple, similar functions in the same space will increase use-per-square-foot efficiency. For instance, a universal approach to outpatient clinic design will allow for multiple specialties to flex up and down, using a series of modules seamlessly. At the largest scale, whole-quad flexibility will allow for massive repurposing of a series of structures, or even provide an exit strategy in case real estate holdings need to be reallocated.
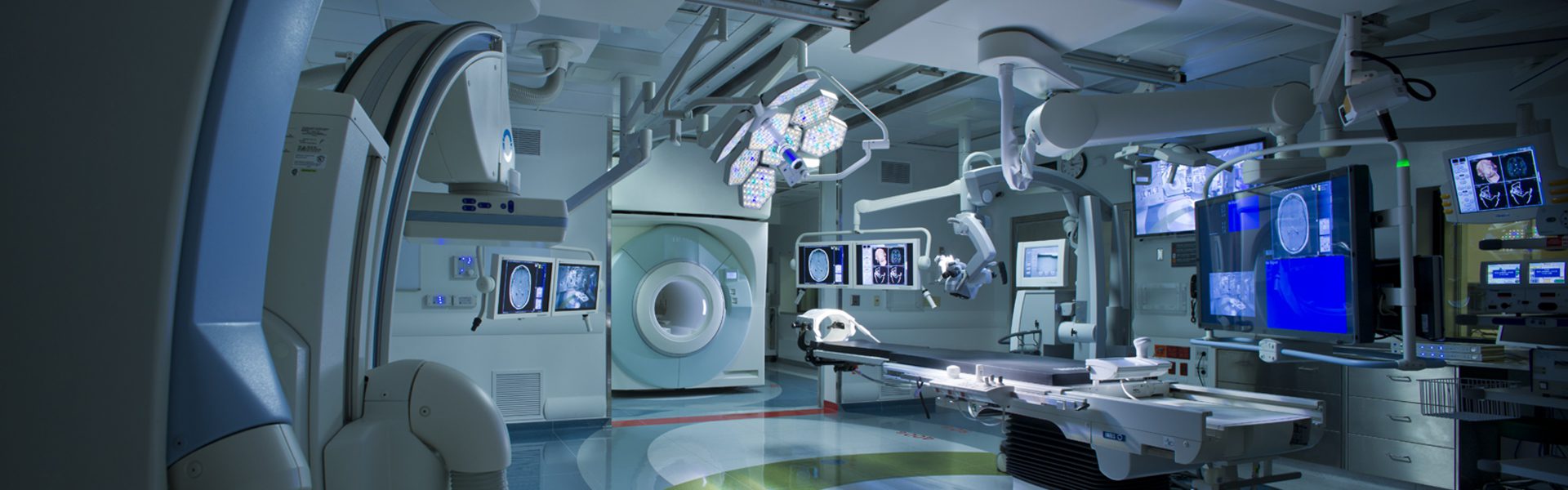
Technology-led Design

Brigham and Women’s Hospital, Advanced Multimodality Image Guided Operating Suite
Ten years ago, technology and information infrastructure represented less than half of the construction budget of a healthcare building, but it was growing. In the future, system integration and information technology will not only represent the largest portion of a building’s construction budget, but will drive its design. Technology is quickly approaching the true “plug and play” level of integration for an entire building. The design community will need to adapt to this coming boom in system integration and plan for a different skill-set on the typical healthcare design team.
Role of Design in a Provider of Choice Environment
The younger generation is more connected. They are more comfortable with information gathering and significant choice decision-making. Ten years ago, our patients went primarily where their physician told them to go, but now, they are looking into options and shopping healthcare. As this trend continues to grow, especially at the Center of Excellence level, health systems will need to invest in elements of choice. In this area, the role of design will have a significant impact. Good design firms will be able to bring tools and experience to the table to help differentiate which elements will be good value and which will be too costly for valued return. This will involve not only experience from past projects, but also knowledge of industry trends and connections to Big Data research.
A retail-type mentality will need to be considered to balance financial constraints with elements of choice. The days of the impressive lobby and grand piano are gone. Spaces that provide a noticeable service will be most notable, and quality environments that respond to human needs will raise patient satisfaction and staff retention. Design will be about measurable results and aesthetic elements that make a difference.
Higher Acuity Levels in More Facilities
While advancements in medicine, technology and treatment will keep more people healthy longer, the ones that will need to be hospitalized will be sicker. They will require a higher level of care for longer periods of time and generate a number of support space challenges. The future of this issue, as it relates to facility impact and design, will be on the adaptability of the design industry to understand this change in acuity across multiple platforms and drive change, in traditional design as well as regulatory agencies, to envision a new breed of healthcare buildings. Care efficiency will be a driver, so traditionally low-acuity environments, such as outpatient clinics, will need care for a higher level of patient to maintain viability. Inpatient zones, usually consisting of an 80/20 mix for intensive-level acuity will need to handle a much higher volume of super-acute patients. Healthy zones, for traditionally simple patient visits, will need to increase efficiency to handle similar volumes but in a more streamlined fashion. All of these changes will require a re-thinking of the standard inpatient/outpatient models. The challenge will demand senior-driven teams of experienced designers, partnered with their clients, dedicating real time to explore design-deliver methods for the future.
Growing Outpatient Care Volumes

University of Massachusetts Medical School, Ambulatory Care Center
The sick are getting sicker, but the population is getting healthier. Advancements in medical care are allowing more and more individuals to seek care in a healthier environment. This is a trend that has spiked in recent years and will continue to grow in the future. The change greatly helps decrease over-crowding in our tertiary medical centers and smaller inpatient hospitals, but has spawned a number of new challenges for a growing outpatient population. First, outpatient care needs to be efficient. It relies on the quality care of a high volume of patients in an environment that feels healthy. These patient’s expectations for a “different and more efficient process” creates a challenge as the market grows exponentially. The challenge of the design community will be to continue to advance this important building type to be more universally flexible and more technologically advanced while continuing to support the efficient business model.
Advancements in patient reception and tracking, along with a higher level of acuity, will create new types of outpatient treatment spaces. Integration with telemedicine concepts will allow for “smart-growth” within the ambulatory network, helping to reduce the physical visit volume. Additionally, design teams will need to consider elements of choice with these facilities as well, given the growing visit volume and importance to the system’s overall business model. Outpatient care, while the most robust of the models moving forward into the future, will have the greatest need for “design re-thinking.”
Facility Repurposing
The change in our industry is extreme, and moving faster every year, but our healthcare facilities and infrastructure are growing older with the passing of each decade. New buildings, while flexible and technology-enhanced, are more expensive than ever, requiring a major financial commitment. To bring our healthcare system as a whole up to world-class, a balance will need to be struck between new SMART construction and the re-use of viable facilities. Simply building a new facility every time a need exists will not be a financially viable option. Design teams will need to adapt by developing new tools, teams and processes for whole building repurposing. This new expertise will take a different approach than traditional renovation.
The repurposed building will integrate the latest technology and IT backbone. It will connect to the system, think like its new counterparts and accept changing equipment. If not, the financial investment, even though smaller than land acquisition/new construction, will be a waste of resources. Structural modifications and mechanical system upgrades will be significant, and good design teams will work with the local regulatory agencies to be adaptable. The industry will find a strong need for true building scientists as these buildings will need to be adapted to perform. This is a challenging undertaking, but given the future need for new healthcare space, it is an essential financial model.
The future of healthcare will take on many different looks depending on your point of view. For the design community, it will be a total re-thinking of the traditional building models, from treatment types to adaptability. How we approach truly flexible buildings to an advanced approach to building re-purposing will constitute a significant shift, not just in the traditional architectural process, but in the way firms create expert teams, approach planning and integrate technology.