In this series, members of our core healthcare team discuss design philosophy and current trends in healthcare design.
Lean Design and Process Improvement has changed the way architects, healthcare practitioners and facility planners think about building performance, space requirements, capital costs and how family centered care is measured, quantified and expressed in programming, planning and design. With the rising cost of healthcare, it is more important than ever to question conventional and anecdotal based schemes and identify design that brings value to our customers. This requires open dialogue about potential issues and the freedom to ask “why?” until the root issues are identified.
For over 50 years, PAYETTE’s approach to design has been about process improvement. In the 1940s and 50s, the founding partners, Frederick Markus and Paul Nocka, began conducting time and motion studies of clinical workflow for their hospitals. These early studies were based on empirical research and had a significant effect on hospital design at the time. Today the firm still continues to pursue and support a process of collaborative inquiry, vigorous dialogue and the synthesis of ideas and techniques.
In the early stages of planning, it is important to look at the hospital within the context of a complex health system and use the goals important to our clients: quality of care, outcomes, patient satisfaction and staff retention to inform the programming and design. PAYETTE’s recently completed project at Boston Children’s Hospital included an addition of 44 inpatient beds, 12 short stay beds, inpatient support and imaging, as well as a satellite pharmacy.
The architectural team spent a significant portion of the planning process working with the clinical support staff, health technology management team, informatics, emergency response team and the planning, design and construction group to understand their specific challenges, as well as identify unnecessary tasks that interrupted the flow of their work and potential quality of care.

Time and Motion Study to Optimize Space and Staffing Needs
Patient Room Mock-Ups

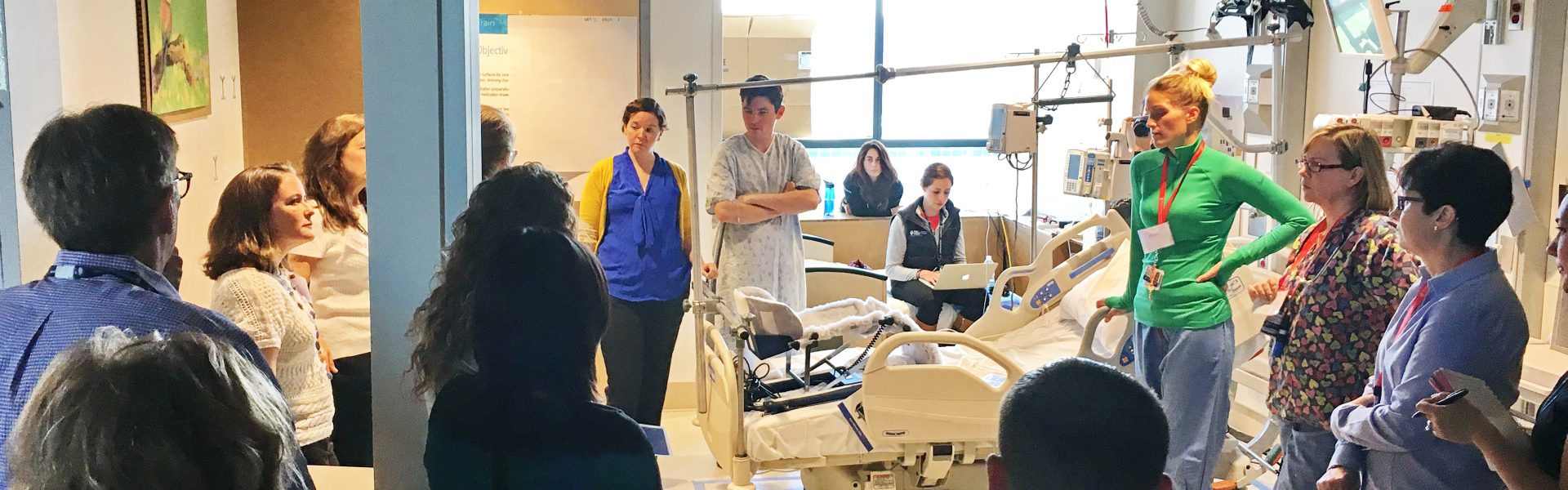
As a part of their process improvement evaluation, the design team created a series of room mock-ups, which simulated real working environments for the staff. The mock-ups allowed staff to see their daily tasks in a new light, question whether the established norm was still relevant for their work and what could be done to improve upon the existing standards. Consequently, the team made changes to the location and configuration of the medical gases in the headwall, relocated the nurse call devices to a more convenient location for the staff, located supply closets directly outside of the patient room, incorporated room side charting, as well as made a host of other architectural modifications to the standard patient room layout. To better accommodate the families of patients the staff, the design team also collaborated to include an integrated wardrobe and activity table inside the patient room.
Discharge Procedure
Another process we reviewed during planning was the discharge procedure for children and their families. The existing process for discharge instructions was often mistimed due to a delay in medical distribution from the pharmacy. The new design included a satellite pharmacy to supplement the main pharmacy. The design team worked with the pharmacists to analyze off shift workflow, modify lines of sight and plan a more efficient layout.
Post Occupancy Evaluation Process
At the close of a project, the staff is often excited about the new space. However, once work begins again and new labor patterns are established, Process Improvement is still an important part of evaluating the effectiveness of the new design. It is our practice to analyze our design through a rigorous Post Occupancy Evaluation (POE) process in which our designers and planners visit our buildings at least a year post occupancy to assess how effective, or ineffective, the implemented design is for the patients, staff and other users of the building. The results of PAYETTE’s studies have allowed the firm to recommend additional improvements to clients on the basis of our empirical research and data.

The POE for the James Mandell Building at Boston Children’s Hospital was completed over a year after occupancy and addressed general questions about how occupants were using the space, whether they were using it as intended, as well as more specific questions about pharmacy workflow and efficiency, room side charting and changes to the headwall. Many of the changes to design and clinical flow incorporated as a result of the early planning mock-up were received with positive feedback. The increase in patient room size and move to single-occupancy patient rooms, from the previous double-occupancy rooms, was warmly received by patients and their families. However, the POE revealed that the move to all private rooms impacted Environmental Services much more significantly than expected.
The private rooms took over twice as long to clean and turn over, which was an additional operational expense. In contrast, the dedicated patient and family areas, which included foot wall tables and chairs incorporated into the patient room design, were noted as very positive additions, and the clinical staff particularly appreciated the isolation supply closets located directly outside of the patient rooms.
The decentralized closets allow staff to collect items such as linens or precautionary equipment without a long walk to a central clean supply room, thus eliminating unnecessary time spent moving through the unit. While a significant portion of time during the mock-up was spent evaluating the location and configuration of the patient room headwall, the POE revealed that there were still staff concerns as to the usefulness of the services provided.
Evaluation of the new satellite pharmacy also garnered mostly positive feedback. Almost two years after opening, the pharmacy had dispensed 7,000 medications, with a peak of 1,000-1,500 medications prepared in a three hour time span. This was a significant improvement over the prescriptions/SF from the main pharmacy.
Recognizing the importance of continuous improvement, PAYETTE is further investigating and incorporating the findings from our POE on additional projects at Boston Children’s Hospital, including PAYETTE’s current Satellite Hospital in Waltham, MA . Currently in the Design Development phase, our team continues to explore the optimal medical gas headwall layout and construction through additional mock-ups and user workshops, comparing fabrication methods and number of gases for efficiency and cost savings. Additionally, the team is working with the staff to add more value to the patient footwall and family spaces within the patient room.