The root of any successful patient care unit is an efficient and effective operational plan developed through rigorous analysis, testing and optimization. This is crucial during the planning process of everything from block diagrams adjacency within the unit to a departmental organization.
Utilizing a robust planning process and design explorations, our healthcare team has successfully designed patient care units for many of our clients including Penn State Health and Beth Israel Lahey Health. During the planning phases of these projects, we focus on two key objectives:
- Thorough analysis of existing operational flow to identify opportunities for improvement.
- Development of a unit layout that fully and efficiently supports the optimized operational flow.
To accomplish this, we use a series of planning processes and tools that can convey ideas, communicate with end users and receive effective feedback. Tools, such as shadow studies, benchmarking, virtual simulations and physical mockups, shape the design of the patient care unit to find the optimal solution tailored to each of our clients.
EVALUATIONS OF CURRENT STATE
Our team has deep knowledge of planning and designing medical intensive care units developed through years of experience. However, we do not assume to know exactly how every institute’s unit is run. Our medical planning teams begin by observing the existing unit in action to thoroughly map existing workflows related to patients, staff and materials. Conducting shadow studies for each shift of each department helps us understand if and how patterns vary through the day and identify any important variations in workflow. The unbiased view that we bring to evaluation and analysis is a valuable tool to establish the basis for the initial visioning sessions, discussion of existing conditions and exploration of different LEAN options.
CASE STUDIES AND BENCHMARKING TOURS
Benchmarking tours of key peer facilities is also crucial to provide a broader view of current practice patterns and operating models. The focus is on an operational analysis and patient care models of peer facilities: why and how does it work, and would their systems work for our current project?
VISIONING & GUIDING PRINCIPLES
Defining fundamental values and guiding principles with the leadership group is critical to the success of a project and ensures clarity for the entire project team. The principles are generated through a complete evaluation of the existing units, tours of new facilities and the understanding of future technologies. A shared understanding of project goals and standards are developed and established to guide the planning and design of the space.
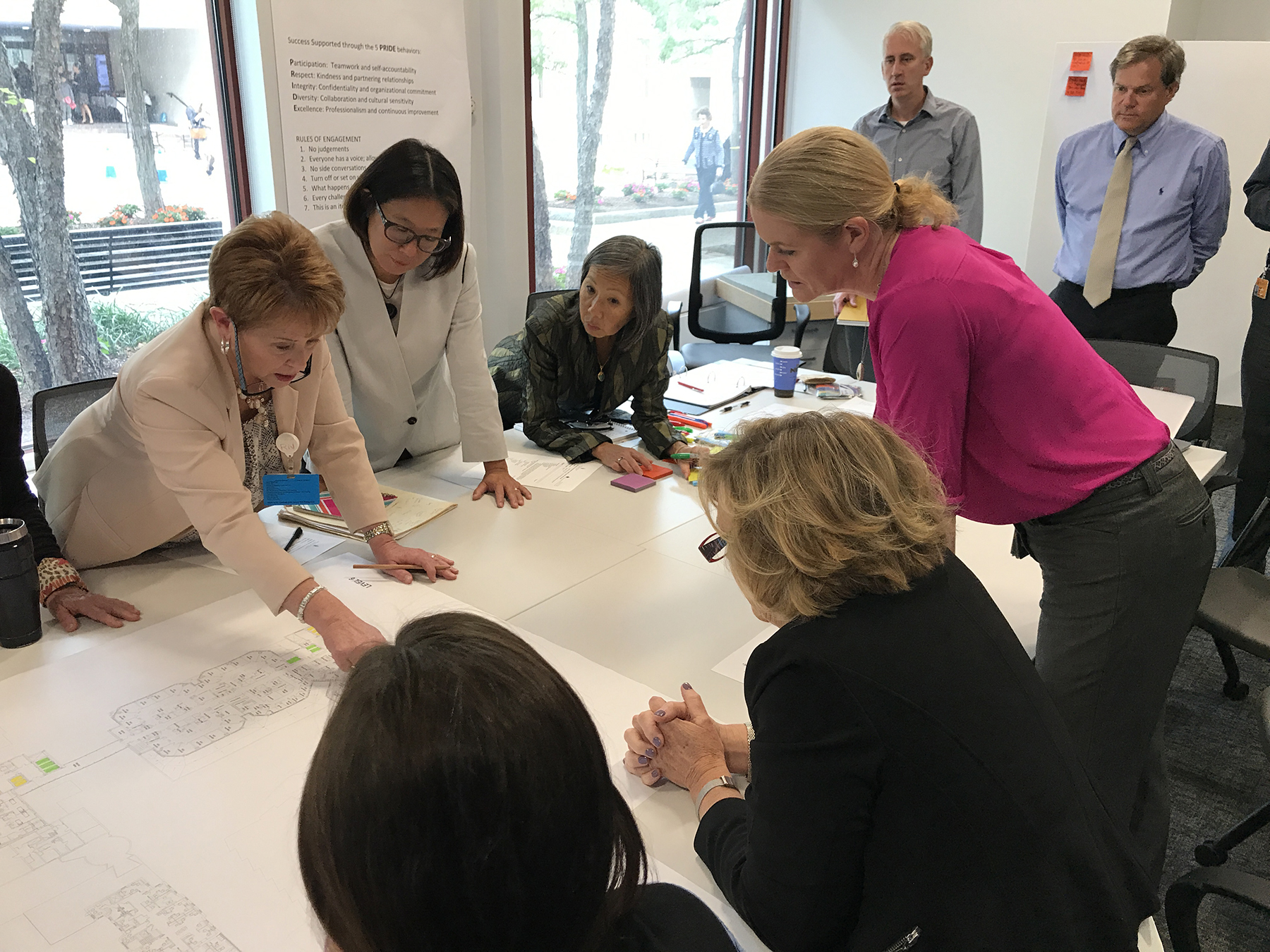
LAYOUT EXPLORATIONS
A thorough concept study exploring every aspect of the plan is essential to ensure we have a complete view of the situation. To help achieve the level of depth, we start with functional programming and overlap with the conceptual study so that each exercise informs the other. Space programs are frequently more useful and understandable when they are graphically represented and tied directly to physical conditions.
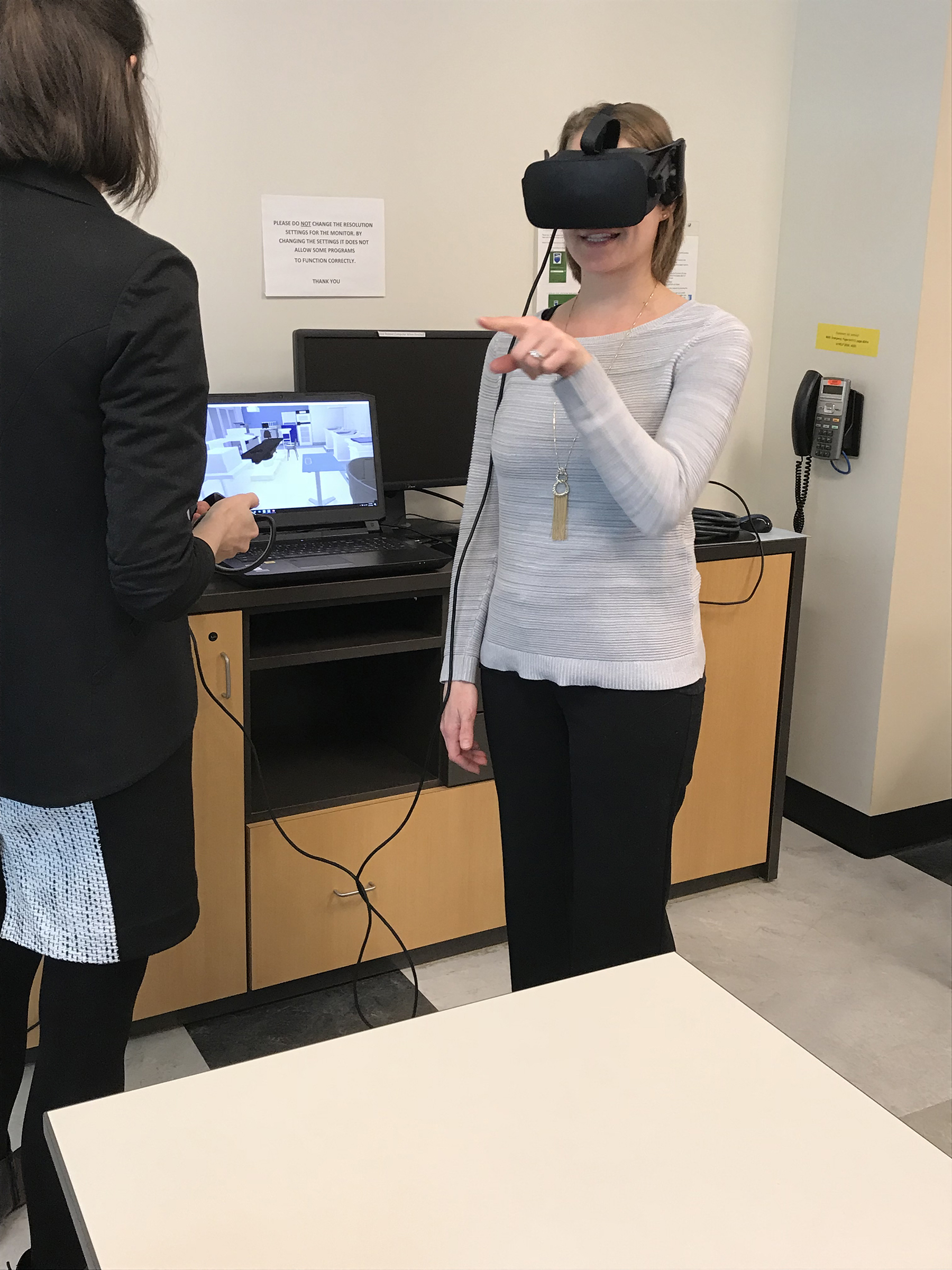
VIRTUAL SIMULATIONS
PAYETTE has the capacity and technology to use virtual reality to model key spaces and create opportunities for users to “walk” through a proposed environment. We currently use simulation systems for design and workflow analysis of our healthcare projects and have found them to be incredibly valuable tools to test, explore and communicate proposed design options. In particular, these tools are tremendously helpful in testing key component orientation and equipment placement (such as early patient room studies) to facilitate the process of locating key pieces of equipment before the construction of physical mockups. It is also a great tool to visualize proposed interiors finishes and to allow caregivers to become familiar with the new environment.
PHYSICAL MOCKUPS
Along with virtual simulations, cardboard final room mockups with finishes confirm the design complies with the project vision. The construction of full scale cardboard mockups for running simulations is a critical step in informing sizes and layouts of patient care and clinical support spaces. We recently built full scale mockups of key spaces for Boston Children’s Hospital, PennState Health and Beth Israel Lahey Health. This gave us the ability to run simulations with equipment in the spaces to evaluate any flow issues. We were then able to optimize the sizes and configurations.

Through this collaborative design process with our clients, we have the ability to develop unique healing environments to positively influence providers and patients.


